Based on international review of existing studies1, these elements are needed to provide support for healthcare workers:
- Quality, accessible PPE for all HCWs to provide security and reduce likelihood of infection for themselves and their loved ones.
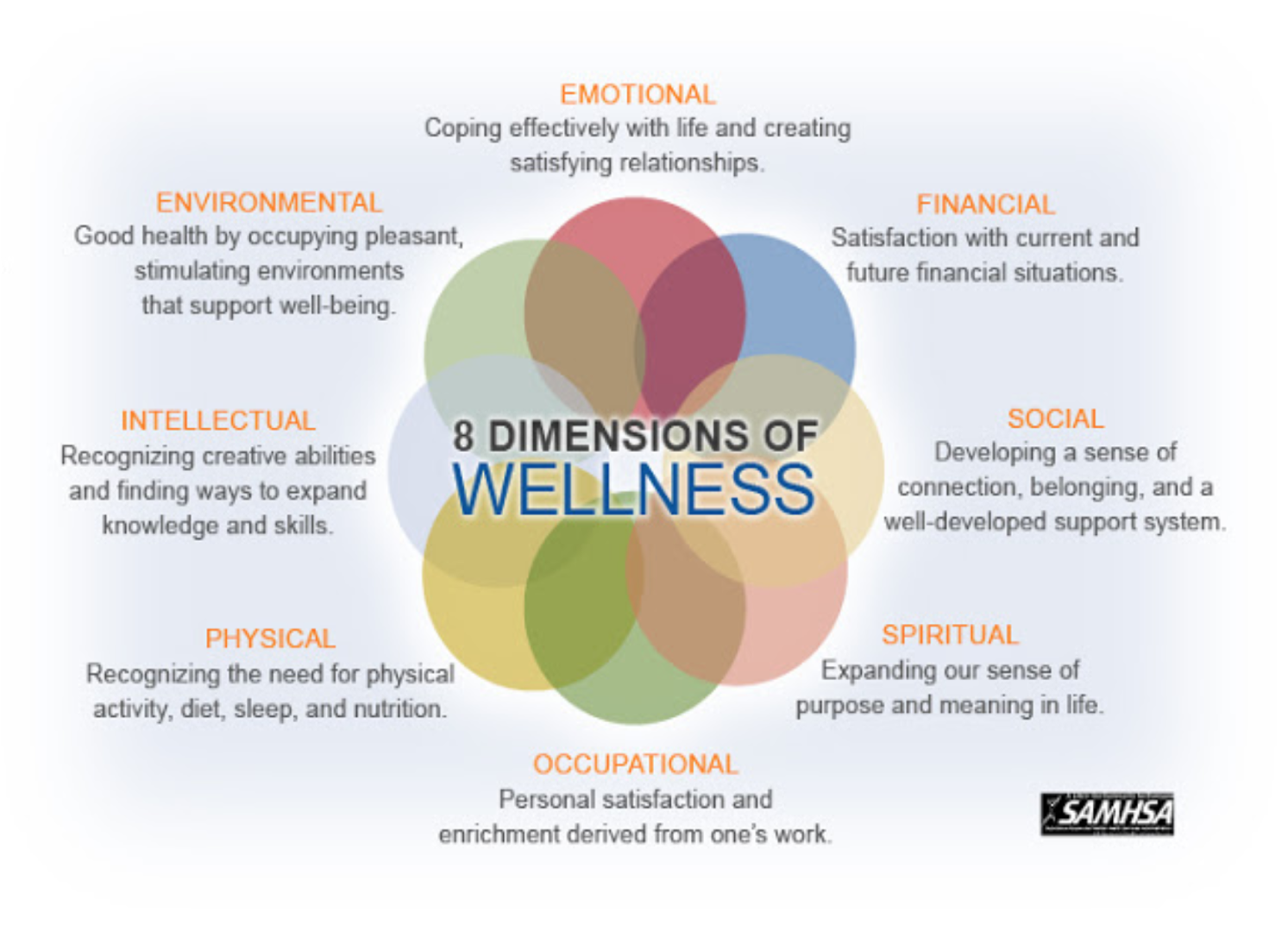
- Individual AND organizational strategies to optimize wellness for healthcare providers in areas of nutrition, exercise, mindfulness, sleep quality, and reducing burnout.
- Short-term and long-term individualized wellness and mental health interventions to address the physical and emotional tolls of COVID-19.
- Immediate and individualized access to psychological first aid mental health resources.
- Opportunities to implement telehealth in a variety of settings to limit exposure to infection.
- Reduce stigma on mental health symptoms and the psychological impact of significant stressful events within HCWs.
- Develop new HCW community groups and encourage participation to allow connections and reduce feelings of isolation.
The need for HCW self-quarantine
OSHA recommended before COVID that healthcare facilities plan for the possibility of separate housing for HCWs in the event of pandemic influenza.
COVID-19 spreads very similarly to influenza, so these same precautions should be implemented.
Because of increased risk of infection, and chance of unknowingly spreading infection to families, HCWs may need to self-isolate.
Those with the ability to do so may isolate at their homes in quarantine rooms.
Many HCW, especially those who are lower tier essential workers, may not have the resources to self isolate and live in multigenerational households with family members at high risk to experiencing a severe case of COVID-19 due to their age or a precondition.
Some have begun camping out in their basements, tents, garages, and tree houses in the backyard.
Needs of HCWs in self-quarantine
Places to isolate and keep family safe are essential. HCW that do not have such spaces need to be supported with safe affordable if not free housing.
In the event of self-quarantine and separate housing of HCWs, it is imperative that these be restful locations with access to adequate meals. This alone is why many at-home situations are less than ideal for HCWs.
Because they are also leaving their families behind, they may also need assistance with childcare or pet care. HCWs may not have a spouse or partner to assist to take on childcare. Their spouses/partners may also be a member of the essential workforce. Pet fosters can reduce worry about pet-care in the event of self-quarantine.
HCW families need support
In addition to needing assistance with childcare and other errands, families of HCWs also need social support.
Studies in China during the height of their COVID-19 outbreak showed that HCW’s families were at increased risk of developing symptoms of generalized anxiety disorder and depression.
Keeping open lines of communication with their HCW family members and providing information to families can help to reduce these mental health impacts.
Assisting in childcare and errands for these families can significantly reduce the impact of stressors from daily basic needs.
Some communities have set up networks where students and volunteers can be assigned to families to assist with errands and babysitting that reduce the impact of HCW self-isolating or maintain long working hours.
Workplace dynamics
Trust in the workplace is essential to HCW wellbeing.
To counteract the potential decline in HCW availability due to fear and anxiety, and to curtail the potential rise of nosocomial infection, it is critical to strengthen HCW safety and trust in the system within which they work.
Workplace Safety is a primary health concern for HCW.
References
1. Shreffler, J., Petrey, J. and Huecker, M., 2020. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health.
Yuchen Ying, Fanqian Kong, Binbin Zhu, Yunxin Ji, View Zhongze Lou, Liemin Ruan, 2020, Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study Now published in BMC Psychiatry doi: 10.1186/s12888-020-02784-w
Center for the Study of Traumatic Stress, Supporting Families of Healthcare Workers Exposed to COVID-19
The Atlantic, “The Child-Care Crisis Is Even Worse for Health-Care Workers”